Clinical Validation of Artificial Intelligence–Augmented Pathology Diagnosis Demonstrates Significant Gains in Diagnostic Accuracy in Prostate Cancer Detection
70% REDUCTION IN CANCER DETECTION ERRORS
The study’s outcomes were pivotal in Paige Prostate Detect ultimately receiving the first FDA-approval for an AI in pathology
CLINICAL VALIDATION OF ARTIFICIAL INTELLIGENCE–AUGMENTED PATHOLOGY DIAGNOSIS DEMONSTRATES SIGNIFICANT GAINS IN DIAGNOSTIC ACCURACY IN PROSTATE CANCER DETECTION
Published in Archives of Pathology and Laboratory Medicine
Patricia Raciti, MD; Jillian Sue, MS; Juan A. Retamero, MD; Rodrigo Ceballos, MSc; Ran Godrich, MS; Jeremy D. Kunz, MSc; Adam Casson, BS; Dilip Thiagarajan, MS; Zahra Ebrahimzadeh, MSc; Julian Viret, MEng; Donghun Lee, MEng; Peter J. Schüffler, DrSc; George DeMuth, MS; Emre Gulturk, MSc; Christopher Kanan, PhD; Brandon Rothrock, PhD; Jorge Reis-Filho, MD, PhD, FRCPath; David S. Klimstra, MD; Victor Reuter, MD; Thomas J. Fuchs, DrSc
Arch Pathol Lab Med (2023) 147 (10): 1178–1185.
ABOUT THIS STUDY
Paige designed this ground-breaking study to understand how assistance from Paige Prostate Detect, an AI that aids in the detection of prostate cancers, could impact pathologist performance in a simulated diagnostic practice.
THE RESULTS
A group of 16 pathologists reviewed 610 prostate needle biopsy whole-slide images first without support from the AI, and then after a washout period, assisted by it. Changes in their sensitivity, specificity, and efficiency were assessed.
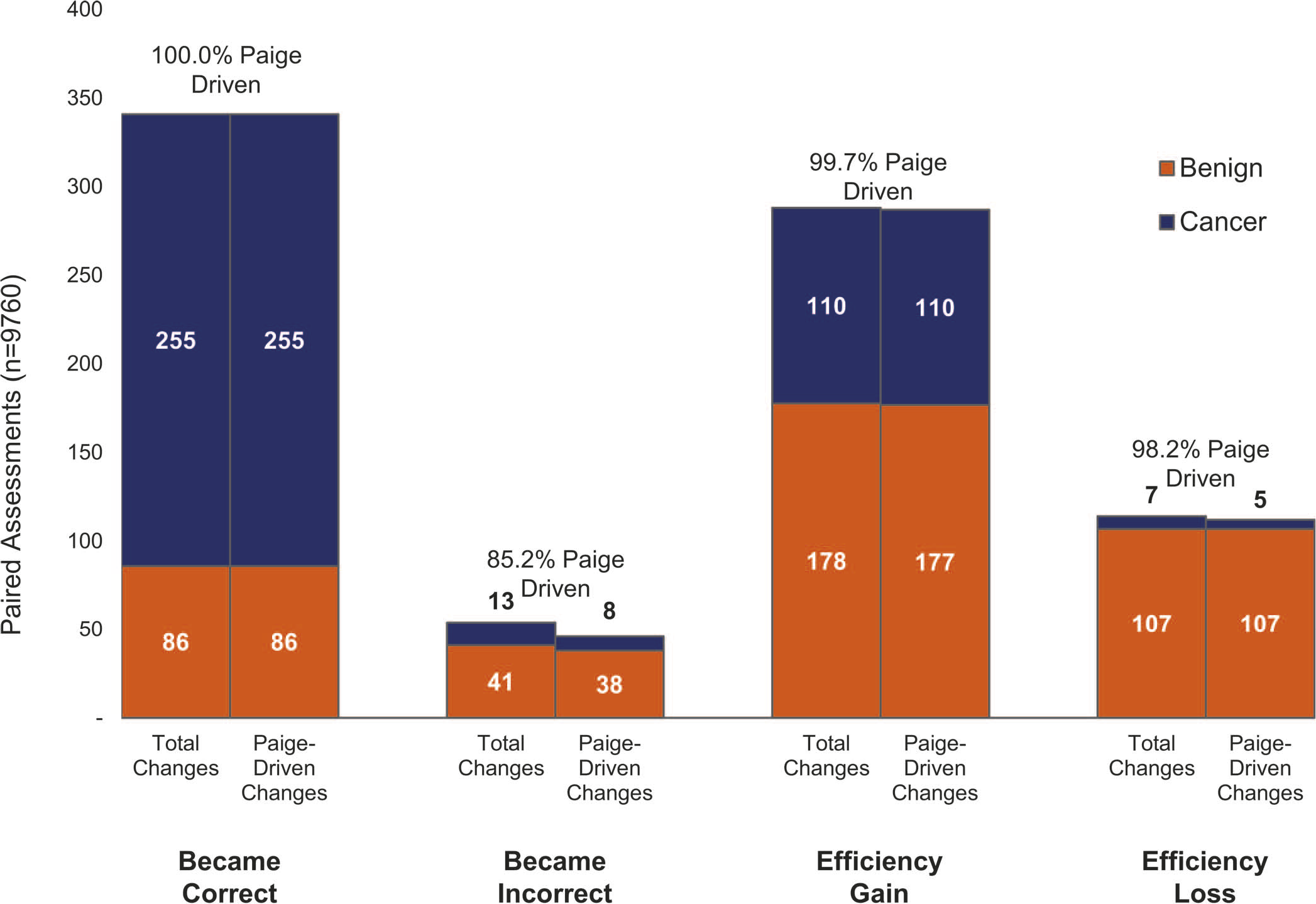
Using Paige Prostate, pathologists improved their sensitivity and specificity across all histologic grades and tumor sizes. Accuracy gains on both benign and cancerous whole-slide images could be attributed to Paige Prostate, which correctly classified 100% of the whole-slide images showing corrected diagnoses in the Paige Prostate assisted phase.
70% reduction in cancer detection errors
97.4% sensitivity for cancer detection | standalone performance
94.8% specificity for cancer detection | standalone performance
Statistically significant sensitivity gains were seen among non-GU pathologists (8.5%) and GU pathologists (3.9%)